Patient Information about Pancreas Cancer
What is pancreas?
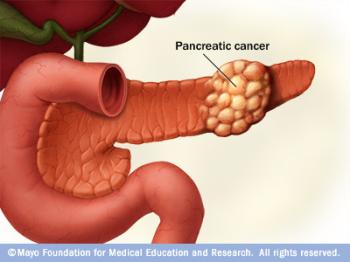
Pancreas is an organ in your abdomen that lies horizontally behind the lower part of your stomach. The pancreas secretes hormones, including insulin, to help your body process sugar in the foods you eat. It secretes enzymes that aid digestion.
What is Pancreas Cancer?
It’s not clear what causes pancreatic cancer. Pancreas cancer occurs when cells in your pancreas develop mutations in their DNA. These mutations cause uncontrolled cell growth which is called “tumor”. Most pancreatic cancer begins in the cells that line the ducts of the pancreas. This type of cancer is called “pancreatic adenocarcinoma”.
What are Signs and Symptoms of Pancreas Cancer?
Signs and symptoms of pancreatic cancer often do not occur until the disease is advanced. When signs and symptoms do appear they may include;
1. Upper abdominal pain that radiates to your back. A growing tumor may press or infiltrate nerves in your abdomen causing pain.
2. Jaundice (Yellowing of your skin and whites of your eyes). Pancreatic cancer that blocks the liver’s bile duct (choledochus) can cause jaundice. Your skin and eye gets yellow, urine gets dark-colored, and stool gets pale-colored.
3. Weight loss may have several reasons; (a) cancer itself causes loss of appetite, (b) tumor pressing your stomach may make it difficult to eat, (c) your body may have difficulty properly processing nutrients from food because your pancreas is not making enough digestive juices.
4. Bowel obstruction occurs when pancreatic cancer presses or invades duodenum (small intestine). In this case nause and vomitting may occur.
How Pancreatic Cancer is Diagnosed?
Imaging Tests to create pictures of your internal organs including your pancreas are essential to diagnose pancreatic cancer. These imaging tests include ultrasound (US), computerized tomography (CT), and magnetic resonance imaging (MRI). These tests not only diagnose a pancreatic tumor, they also show the stage of pancreatic cancer (if you can be operated or not).
Blood Tests for specific proteins shed by pancreatic cancer cells (Tumor markers) are also helpful in diagnosing pancreas cancer. CA 19-9 is the tumor marker for pancreatic adenocancer, but it is not always reliable.
Biopsy is the procedure in order to obtain definitive diagnosis of pancreas cancer. It is a procedure to remove a small sample of tissue from the pancreas for examination under a microscope. A biopsy sample can be obtained by inserting a fine-needle through your skin and into your pancreas under the guidance of computerized tomography (CT-guided biopsy).
What are Stages of Pancreatic Cancer?
Using information from tests, your doctor assigns yor pancreatic cancer a stage. The stages of pancreatic cancer are:
Stage I. Cancer is confined to the pancreas.
Stage II: Cancer has spread beyond the pancreas to nearby tissues and organs and may have spread to the lymph nodes.
Stage III. Cancer has spread beyond the pancreas to the major blood vessels around the pancreas and may have spread to the lymph nodes.
Stage IV. Cancer has spread to distant sites beyond the pancreas, such as the liver, lungs and the lining that surrounds your abdominal organs (peritoneum).
What is the Treatment of Pancreatic Cancer?
The treatment for pancreatic cancer depends on the stage and location of the cancer as well as your age, overall helath and personal preferences. The first goal of pancreatic cancer treatment is to eliminate the cancer (with surgery), when possible. Pancreatic cancer typically spreads rapidly and is seldom detected in its early stages. It has often a poor prognosis, even when diagnosed early. Approximately %80-95 of patients with pancreatic cancer can not be operated because of the advanced stage at the time of diagnosis. In advanced pancreas cancer whom the surgery can not be performed, doctors focus on preventing the cancer from growing (chemotherapy and radiation therapy) and relieve symptoms to make you as comfortable as possible (bile duct stenting in order to relieve jaundice and celiac ganglion blockage to relieve your pain).
What is the Role of Radiology in Pancreas Cancer?
Detecting pancreatic tumor: Radiology (diagnostic imaging) uses equipments (such as ultrasound, computerized tomography and magnetic resonance imaging) to see your internal organs. Patient with symptoms and signs of pancreatic cancer (such as jaundice, abdominal pain, weight loss) is first referred to a Radiologist. So the Radiologist is the first doctor who “sees” your tumor in your pancreas on CT, US, or MRI.
Staging of pancreas cancer: is done with imaging studies performed by a Radiologist. After staging of the disease, your treatment options are determined.
Needle Biopsy is performed by an Interventional Radiologist. Needle Biopsy is performed under CT guidance. Biopsy is essential for the definitive diagnosis of pancreatic cancer.
Biliary Stent Placement: In patients with advanced stage of the disease (%80-95 of patients with pancreas cancer), Percutaneous Transhepatic Cholangiography (PTC) and Biliary Stent Placement is performed in order to relieve jaundice caused by pancreas cancer blocking the liver bile duct. This procedure is performed by an Interventional Radiologist in angiography suite. A tiny needle is inserted in your liver and bile ducts under sedation and analgesia. Then the obstructed bile duct is “opened” inserting a stent (metallic tube). Interventional Radiologists place a self-expanding metallic stent which is reaches to a diameter of 10 mm after placement into the bile duct. Unlike the plastic tube with a small-diametered lumen inserted by Gastroenterologists under endoscopy, this metallic stent has the great advantage of not getting obstructed later in the later course of disease.
Celiac Ganglion Blockage: is a procedure performed by an Interventional Radiologist in order to relieve your abdominal pain. In advanced cases of pancreatic carcinoma, cancer cells invade nerves in your upper abdomen and causes pain. This pain can not relieve with analgesic medications (pain relieving drugs). In this situation, a needle is placed into your celiac ganglion under CT guidance and alcohol is injected to the nerves. This procedure stops the nerves from sending pain signals to your brain.
Three Interventions in Pancreatic Cancer:
1. For definitive diagnosis : Needle Biopsy (CT-guided FNA)
2. Relieving Jaundice : Percutaneous Biliary Stenting
3. Relieving Pain : Celiac Ganglion Blockage (CT-guided)
In summary, Radiologist diagnoses and treats your pancreatic carcinoma if surgery could not be performed due to your advanced stage of disease.

